 |
 |
Data source: Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov)
SEER*Stat Database: Incidence - SEER 9 Regs Public-Use, Nov 2004 Sub (1973-2002),
National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics
Branch, released April 2005, based on the November 2004 submission.
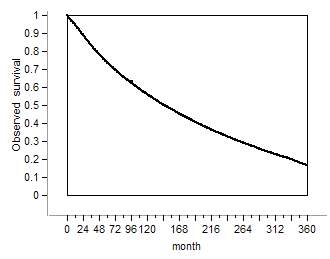
It obviously declines, yet what is less obvious how it declines! From
the third year and onward the slope of the curve continually declines.
In other words, the magnitude of this decline declines with time. This cumbersome
sentence means that breast cancer hazard rate declines. In other words, the
longer a patient lives the better her chances to survive! Yet this optimistic
message may be deduced solely from hazard rates,
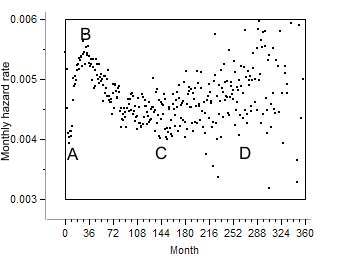
Bi-modal hazard BMH
The survival curve smooths out variation and hides a pattern of great consequence.
The hazard rate is bi-modal. Initially it rises then declines
to rise again. This pattern is called here bi-modal hazard (BMH).
It is unique to cancer and does not appear in other chronic
diseases. It is an epidemiological hallmark of cancer. It is so typical of
cancer that it distinguishes cancer from other chronic diseases.
Cancer proceeds through two phases, compensated, when the tumor does
not cause any damage or distress, and de-compensated, when the patient suffers.
BMH is more pronounced in compensated cancer. The earlier cancer is detected
the more distinct is BMH. In breast cancer it is most pronounced and far less
distinct in lung cancer since when detected it is decompensated.
Some of the hazard rate estimates smooth out variation and obscure BMH. The
present studies apply hazard rate fractions:
HR = #died / (#live at start of the interval - #lost to follow up)
BMH has other epidemiological manifestations:
1. The relapse rate
following breast cancer surgery is bi-modal.
(Retsky et al.(1)).
2. The hazard rate of the first breast cancer recurrence
is bi-modal (Karrison et al (2).
3. Annual hazard rates of recurrence
for breast cancer after primary therapy are bi-modal (Saphner et al (3))
4. Mammography paradox: The hazard
following mammography of young females is higher than in controls Cox
(4).
5. Hazard
rates of recurrence following diagnosis of primary breast cancer
Jatoi et al. (5)
6. Hazard rate of recurrence of breast
cancer in 3811 spanish patients.
7. BMH is pronounced after radiation which destroys the tumor more efficiently
than other treatments.
7a Genital cancers 7b Lung cancer
-- These epidemiological manifestations of breast cancer originate in one
and the same phenomenon: BMH
-- They are linked to cancer detection and treatment. They indicate a potential
iatrogenesis.
-- Since bi-modal hazard rates appear in other cancers, e.g. colon, skin
melanoma and prostate this phenomenon is common to all cancers. In other
words it is an epidemiological phenomenon unique to cancer.
-- In cancers that are diagnosed relatively late, e.g.,
lung cancer, the ascending portion of BMH is missing and their hazard
rate declines.
The descending portion of BMH appears in all cancers and does not
appear in other chronic diseases.
Medical significance of BMH (portrayed in the above figure)
1. AB segment: Hazard rises due to treatment.
2. BC segment: The declining hazard indicates that with time
the patient resists cancer better and better. The longer she lives the better
her chances to survive. The nature of this resistance is the major concern
of this web-site. Although treatment also contributes to this decline, it
appears in untreated breast cancer and in patients
who were treated only once and not treated again
later on
3. CD segment: Marks the final decline when resources are
depleted and illness overpowers the patient.
Hypothesis
These observations convinced me to propose the following hypothesis.
Cancer is a metabolic deficiency caused by a deficiency of
a yet unknown metabolite A. In order to replenish the missing metabolite the
organism grows a tumor which produces a substitute B. Since
the deficiency continually aggravates, the tumor has to grow more and more
in order to replenish the missing metabolite. In advanced deficiency tumor
destroys vital functions and finally kills the patient. Tumor ablation
aggravates the deficiency and the hazard rises. Patients with micro metastases
are protected from therapy induced total ablation and their hazard rate declines.
Clinically this deficiency is manifested by a wasting disease which starts with weight loss and gradually turns into overt cachexia It is named here pernicious cachexia. The tumor protects against cachexia.
Treatment objectives: Do not treat unless the tumor causes
pain and distress or destroys vital functions. Wait as long as cancer is compensated
and treat only during decompensation.
Some detailed studies:
1. Tumor ablation in compensated breast cancer raises
its hazard rate.
2. This phenomenon is observed also in other cancers
and in prostate cancer
3. Bi-modal hazard rate in untreated breast cancer
4. A simple model of breast cancer 4a A
Gompertz model of bi-modal hazard rates
5. Relapse rate following surgery. 5a
A simple model of relapse rate
6. Treatment promotes cancer
progression
7. Conditional Survival
8. Tumor dependency
9. Radiation induced hazard in genital
cancers
10. Radiation induced hazard in lung cancer
11. In advanced age cancers progression is slower
than in young patients.
12. Despite rising breast cancer age adjusted incidence
rate its biology did not change.
13. Long survival with micrometastasis
Farewell my breast
References
1. M. Retsky, R. Demicheli and W. J.M. Hrushesky
Does surgery induce angiogenesis in breast cancer?
Indirect evidence from relapse pattern and mammography paradox International Journal
of Surgery Volume 3, Issue 3
, 2005, Pages 179-187
2. Karrison TG,. Ferguson DJ, Meier P. Dormancy of mammary carcinoma after
mastectomy
J. National Cancer Institute, (1999) 91 : 80-85.
3.
Saphner T, Tormey DC, Gray
R.
Annual hazard rates of recurrence for breast
cancer after primary therapy
J Clin Oncol 1996; 14: 2738-2746.
4. Cox B, Variation
in the effectiveness of breast screening by year of follow-up, J Natl Cancer
Inst Monogr 22 (1997), pp. 69–72
5. Ismail Jatoi , Anna Tsimelzon , Heidi Weiss , Gary M. Clark and Susan G.
Hilsenbeck
Hazard rates of recurrence following diagnosis of primary breast cancer
Breast Cancer Research and Treatment 2005; 89: 2; 173-178